CAR T-Cell Therapy – Revolutionizing Medical Science
Published on 06 Feb, 2023
Chimeric antigen receptor (CAR) T-cell therapy has come to fore as a breakthrough in cancer treatment, specifically for blood cancer. Several companies have invested in it and many treatments have already received FDA approval. Although there are certain limitations to this therapy, they can be overcome via research. The CAR T-cell therapy can not only become a revolutionary treatment for cancer but also cure autoimmune diseases and viral infections.
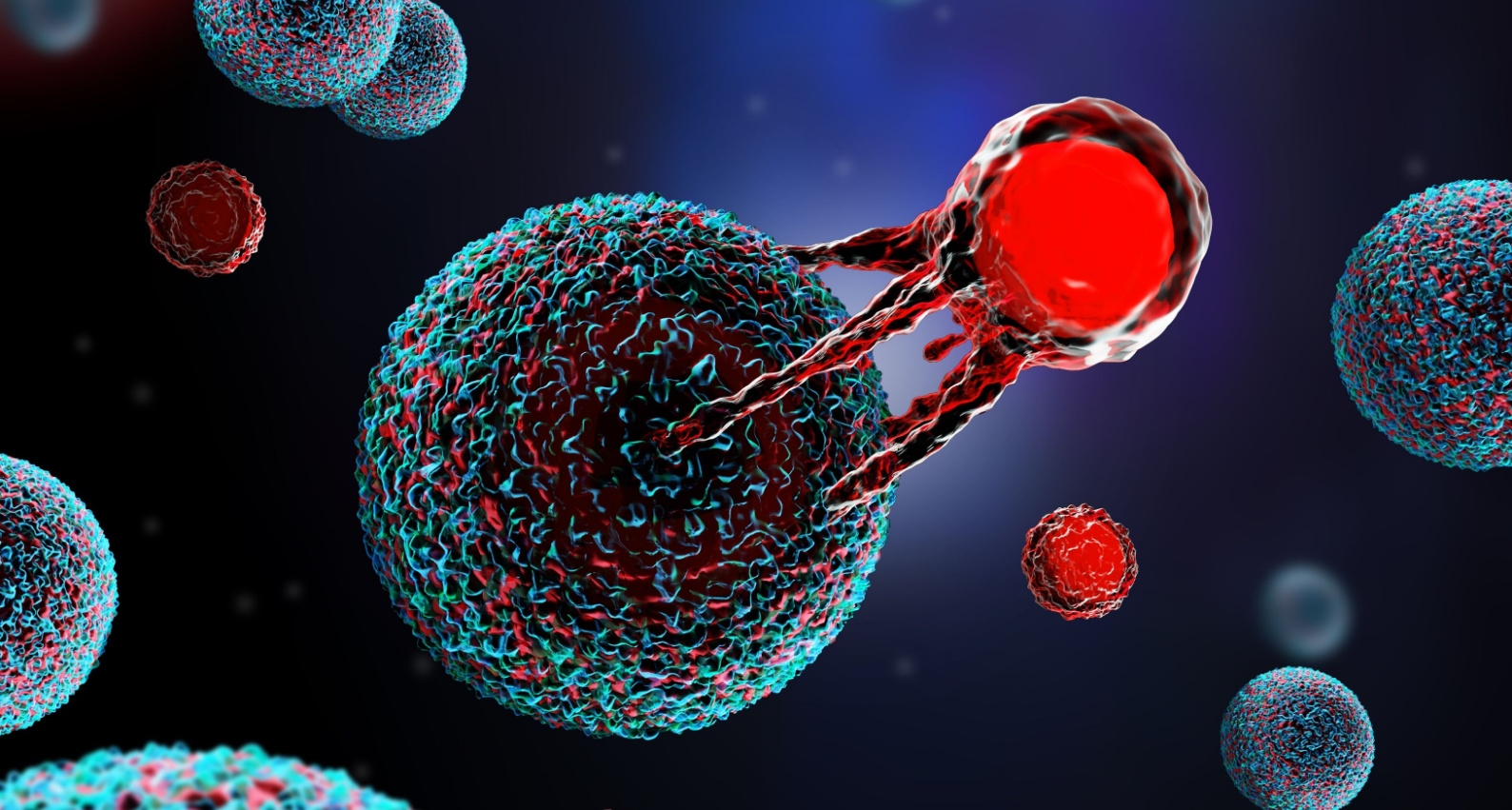
Modern medicines and therapies based on technological advancement in medicine are helping fight critical diseases such as cancer. CAR T-cell Therapy, a cancer immunotherapy treatment, is a method that has proven successful. It uses altered immune cells (T cells) enabling them to locate and destroy cancer cells more effectively.
In their original form, T cells are white blood cells in human body and maintain the body’s immunity. Each T cell contains a receptor that can identify antigens, which are components of foreign entity, that the immune system can identify and destroy. However, at times, cancer cells have ambiguous antigens that are difficult to identify. Hence, the immune system may not send T cells to fight them. This is where CAR T-cell therapy has an advantage. The cells are engineered and given a new receptor that can bind to specific cancer cells and attack them.
Though still in a nascent stage, the CAR T-cell therapy global market size is expected to rise from USD 1–2 billion in 2020–21 to USD 15 billion in 2027–28. Currently, many treatments in this field received approvals in Europe, China, Australia, Singapore, and the UK. Main players in this market are Novartis AG, Kite Pharma, Bluebird, Celgene, and Pfizer. Some key start-ups that have entered the fray are Cabaletta Bio, Be Bio, ImmPACT Bio, and Allogene Therapeutics.
Following are some notable collaborations encouraging the development of CAR T-cell therapy:
- In December 2022, Kite entered a strategic collaboration with Arcellx and acquired Tmunity Therapeutics to pursue CAR T-cell therapy advancements.
- In November 2022, AstraZeneca acquired Neogene to create more cancer-fighting cell therapies. Neogene specializes in discovering, developing, and manufacturing next-generation T-cell receptor therapies (TCR-Ts) to cure solid tumors.
Structure
The CAR T-cells have an ectodomain that includes antigen-binding and spacer domains. There is a transmembrane domain acting as an anchor to T cell membrane and endodomain or intracellular domain that triggers the signaling cascade. Currently, four generations of CAR-T cells exist, and fifth-generation CARs is under active development depending upon the organization of their intracellular signaling domain.
- First-generation CARs comprised a single CD3 ζ- chain or FcεRIγ intracellular domain.
- Second-generation CARs contained single additional cytoplasmic domains, such as 4-1BB, CD28, or OX-40, with the ability to send out a secondary signal if it encounters a tumor antigen.
- Third-generation CARs contained multiple costimulatory signaling domains within the endodomain.
- Fourth-generation CARs had their premise in second-generation constructs. However, the main add-on was a constitutive or inducible expression cassette with a transgenic protein such as a cytokine.
- Fifth-generation CARs are underway and will integrate an additional membrane receptor such as IL-2 or switch receptors.
Process
CAR T-cell therapy is a complex process and takes a few weeks to be completed. The process includes collecting T cells from blood, engineering them in the lab, multiplying them and once sufficient, infusing them back in the body.
CAR T-cell therapy is an intricate cell engineering process. The T cells need to be modified so that they focus on the harmful substance (cancer cells) present in the body. To achieve this, a protein, CAR, is added to the cell’s surface. CAR is a combination of three proteins; one protein that identifies antigens present on cancer cells and attaches itself to it and two proteins that signal the T cell to attack.
Activated CAR T-cells multiply and alert other immune system components to travel to the cancer cell's location. The signaling proteins are called cytokines. Following considerable inflammation concentrated on the cancer cell brought on by these cytokines and activated T cells, the cancer cell eventually perishes. The cancer may go into remission, which indicates that it has either temporarily or permanently disappeared, if all cancer cells are eliminated.
Side Effects and Limitations
There are certain side effects of CAR T-cell therapy. Cytokine release syndrome (CRS) is a serious complication, in which CAR T-cells may trigger release excessive cytokines. High levels of cytokines can cause the immune system to become overactive, resulting in inflammation and a wide range of other undesirable symptoms.
Apart from this, the therapy may damage the nervous system and cause the following:
- Tremors or seizures
- Mind confusion
- Loss of consciousness
- Balance issues
- Trouble in speaking
CAR T-cell therapy specialists are usually able to handle the side-effects successfully.
The treatment has other limitations:
- Exhaustion of T cells
- Limited CAR T-cell persistence
- Bottlenecks in the manufacturing of autologous products
However, with CRISPR-Cas9-based gene editing, overcoming some of these shortcomings is possible. Other drawbacks of this therapy are high cost and limited skilled professional.
On-market CAR T-cell therapies
Currently, CAR T-cell therapy has received FDA-approval for treatment of certain hematological malignancies such leukemia, lymphoma, multiple myeloma. The companies and their treatments with the launch price for one-time treatment are listed below:
- Kymriah (tisagenlecleucel), Novartis Pharmaceuticals, $475,000
- Yescarta (axicabtagene ciloleucel), Kite Pharma, $373,000
- Tecartus (brexucabtagene autoleucel), Kite Pharma, $373,000
- Breyanzi (lisocabtagene maraleucel), Bristol Myers Squibb, $410,300
- Abecma (idecabtagene vicleucel), Bristol Myers Squibb, $419,500
- Carvykti™ (ciltacabtagene autoleucel), Janssen Biotech, $465,000
While FDA has approved these treatments, it is limited for patients who received at least one traditional therapy earlier due to the serious side effects around CRS and ICANS.
Future Potential
CAR T-cell therapy currently focuses on certain types of cancer and has the potential for wide scale applications:
- Research groups in this area suggest that it could be effective in treating autoimmune diseases such as Lupus. This could be achieved with monoclonal antibodies.
- The onset of COVID-19 prompted investment and research to check the effectiveness of T-cell therapies in viral infection treatment. Diseases such as COVID-19 and HIV are being targeted by cell therapies, and certain therapies, such as anti-HIV CAR-T cell therapy, are in the clinical trial stage while others, such as HBV and HCV, are in preclinical development.
- Health researchers from US Davis are researching ways to use CAR T cells and control the HIV by targeting HIV cells without medication. Researchers from University of California San Francisco (UCSF) are conducting a clinical trial in therapies, which modify the patient’s immune cells to treat and eliminate HIV.
Conclusion:
Like every new technology, CAR T-cell therapy has faced doubts and skepticism. However, its soaring success rate has attracted investments in this segment and pushed the regulatory bodies to develop suitable frameworks. Due to innovations and increasing scale of applications, this industry is expected to grow. T cell therapy has the potential to eliminate several types of cancers and represents a significant breakthrough in medical science.

